The Six Sigma model is a continuous improvement approach that has a proven commercial pedigree that can be traced back to the quality revolution of the 1940’s.
Contents
Introduction
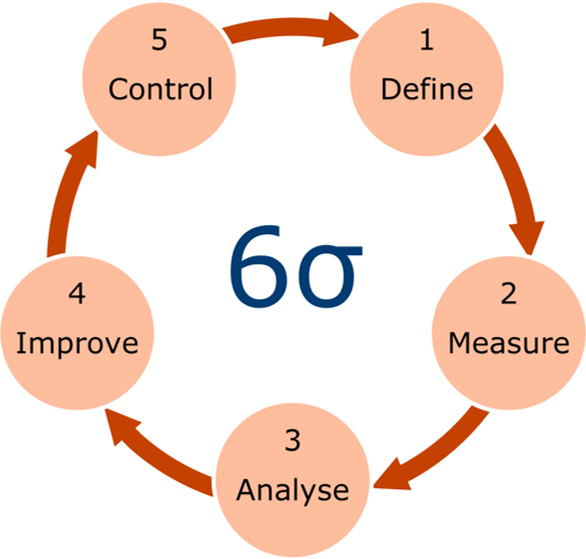
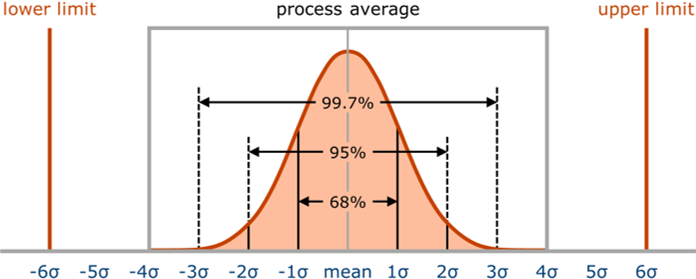
Six sigma is an approach to improvement developed at Motorola in the 1980s, which focuses on removing the causes of defects and reducing variation in processes. It has a meticulous focus on understanding wide-ranging customer needs, prioritising these and designing processes and systems to deliver to those needs. Its purpose is derived from the desire to achieve a performance level equivalent to a defect rate of 3.4 defects per million opportunities. Six sigma uses a disciplined and systematic approach to look at the improvement journey from a number of related perspectives: define; measure; analyse; improve; and control (DMAIC).
Six sigma is typically a facilitated process where experts use qualitative and quantitative techniques to drive process improvement. Although the tools themselves are not unique, the way they are applied and integrated as part of a system is. Six sigma professionals undergo extensive training to be able to select and use tools to evaluate a process from various perspectives and determine which activities are to be improved. It has been embraced by a number of US companies, while application in the UK health system is more limited1.
Six sigma tools help to:
- define a problem, improvement opportunity or requirements
- measure process performance
- analyse processes to determine root causes of variation, defects or poor performance
- improve process performance by addressing root causes
- control the improved process and future performance.
The principles of six sigma are fundamentally based on a statistical approach to process control which limits unnecessary variation in performance, and it is increasingly used in conjunction with lean thinking2.
Footnotes
- Lessons for Lean in Healthcare from Using Six Sigma in the NHS. Proudlove, Moxham and Boaden, Public Money and Management, 28(1):27-34, 2010.
- Lean Six Sigma: some basic concepts. Bevan, Westwood, Crowe and O’Connor, NHS Institute for Improvement, 2013.
Getting Started
Define
The first stage of the six sigma process involves clarification of the project opportunity, creation of the team, definition of the problem aim and scope, identification of the users and stakeholders, description of measures of success, and agreement of the major milestones. Particular importance is given to the voice of users and stakeholders, and its translation to critical-to-quality (CTQ) trees which illustrate how their needs map to actionable system performance requirements, and facilitates understanding about the current processes and opportunities for improvement. Potential benefits to the users and stakeholders are also considered in the light of the resources and time required to deliver such improvement.
Measure
The second stage establishes the detailed requirements and techniques for measurement of the current system performance, in order to capture a true picture of the process. This will include the identification of measures of variance and different types of data, definition of key process input and output variables, development of a data collection plan, and an initial system analysis on data collected.
Analyse
The third stage focuses on the detailed analysis of system performance data, examination of different sources of variability, determination of cause and effect relationships and root causes of problems, and identification of specific opportunities for improvement.
Improve
The fourth stage involves creative thinking and the generation of improvement concepts that address the root causes of the variations and problems observed. These concepts are subsequently evaluated, prioritised, piloted and implemented. A future-state system process map is used to visualise the impact of the proposed changes, identify the gaps between the current and future states, and enable risk assessment of the proposed system. Cost/benefit analysis and planning for full-scale implementation are also undertaken at this stage.
Control
The final stage focuses on institutionalising and controlling the improved processes. This includes process monitoring, preparation of training documents, control and reaction plans, and documentation of before and after results and updated process maps.
Comparison
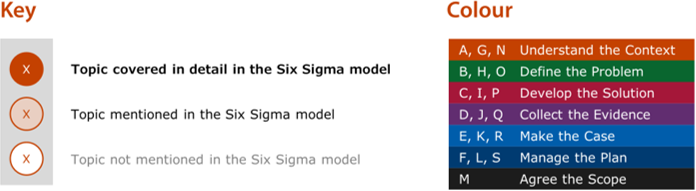
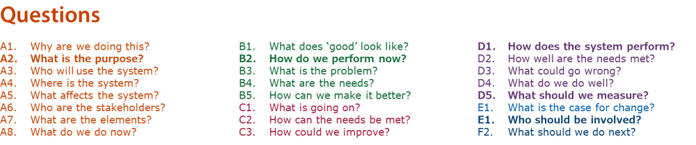
The questions, activities and tools from this toolkit can be mapped to the Six Sigma model of improvement to better understand the relative coverage of the two approaches. Resource material for the Six Sigma model has been analysed in detail to ascertain how it relates to the systems approach in this toolkit, both in terms of the mention of common topics and in terms of the provision of detailed descriptions or advice relating to the same topics.
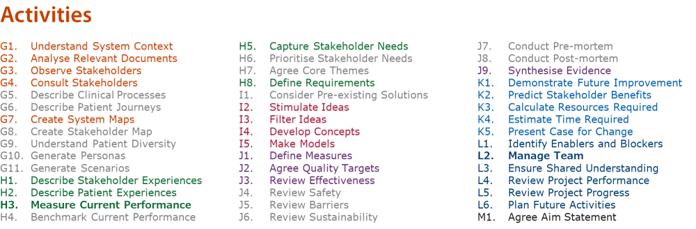
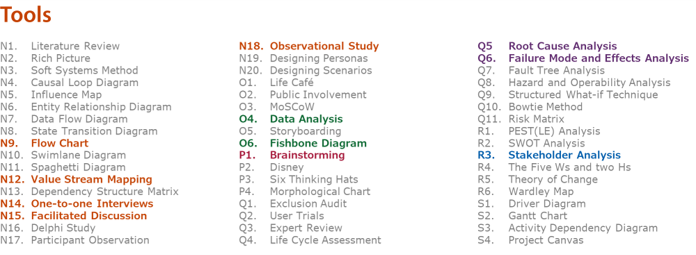
Questions, activities and tools that have particular potential to add value to the Six Sigma model:
Footnotes
Concentric rings diagrams for each aspect of the six sigma model
Feedback
We would welcome your feedback on this page:
Privacy policy. If your feedback comments warrant follow-up communication, we will send you an email using the details you have provided. Feedback comments are anonymized and then stored on our file server
Read more about how we use your personal data. Any e-mails that are sent or received are stored on our mail server for up to 24 months.